SEVERE EPIGASTRIC AND LEFT UPPER QUADRANT PAIN RADIATING TO THE SHOULDER - DIAGNOSIS
Ultrasound reported the appearance of pneumoperitoneum and suggested a CT to further investigate.
The patient was admitted to her local NHS hospital and CT Abdomen/ Pelvis with contrast was performed.
The report confirmed the presence of a small amount of free intraperitoneal gas anterior to the liver and below the left hemidiaphragm. Additionally, there were two ill-defined rounded masses with peripheral enhancement, low attenuation centres and some adjacent streaky perilesional soft tissue at the left gastrocolic ligament and abutting the lateral left hepatic lobe and left hemidiaphragm. The CT report concluded these soft tissue abnormalities were abscesses secondary to recent gastric perforation with a differential of disseminated malignancy.
The patient was treated conservatively in hospital with IV antibiotics for 4 days.
An endoscopy was performed a few weeks later demonstrating a perforated ulcer which had healed itself. The likely cause was thought to be aspirin the patient was taking when on her travels.
A follow-up CT a few weeks later showed complete resolution and no surgery was required.
CT views demonstrating two small pockets of intraperitoneal free gas anterior to the left lobe of the liver as indicated by the green arrows.
 |
Figure 4 |
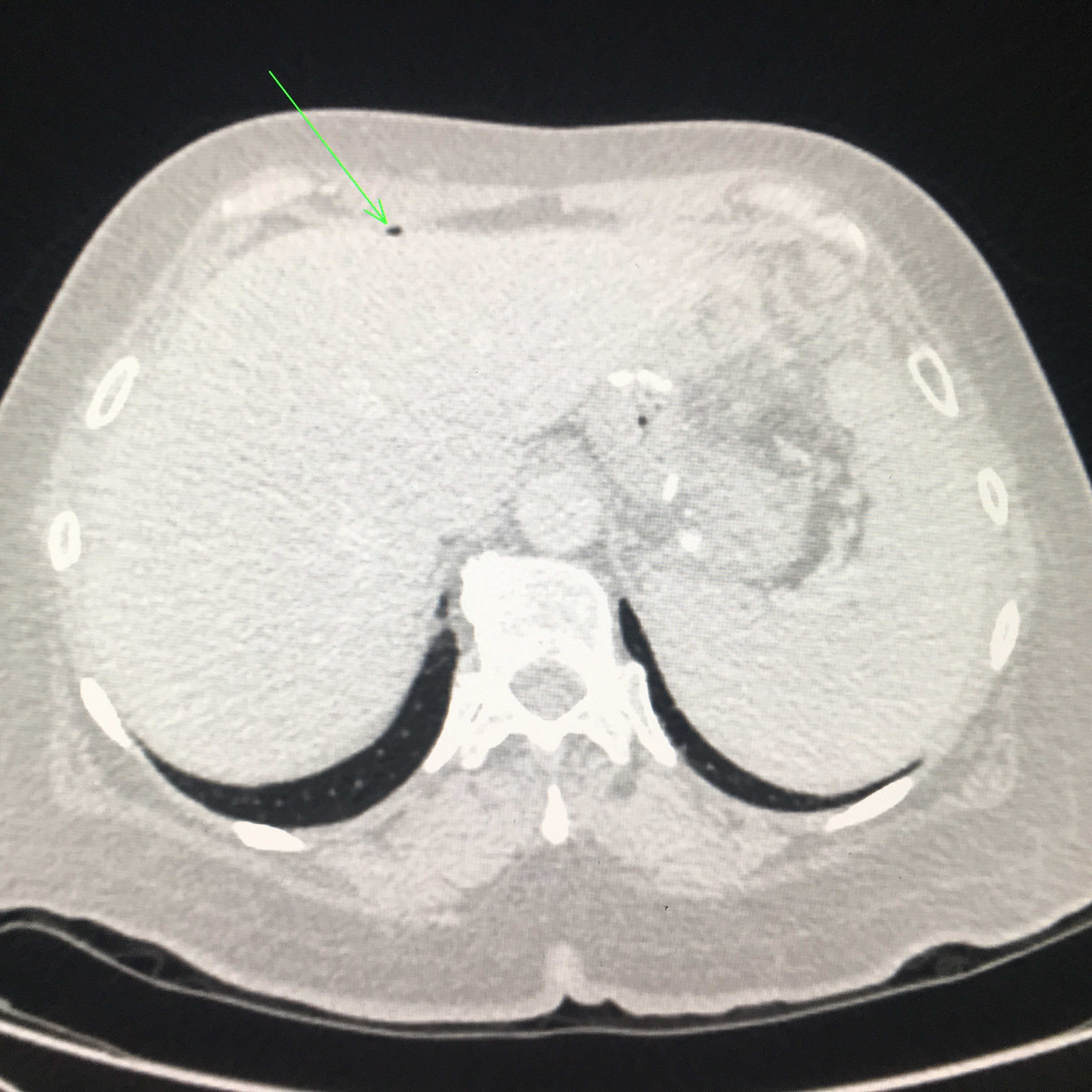 |
Figure 5 |
DIFFERENTIAL DIAGNOSIS
Differential diagnosis of clinical presentation:
There are a range of possible conditions associated with this clinical presentation which include cholelithiasis, cholecystitis, pancreatitis, hiatus hernia, and gastric cancer. Diagnosis can be difficult with history and physical examination alone therefore ultrasound is a useful first-line investigation tool. If the study is unremarkable, a CT scan is indicated to further investigate the regions not accessible with ultrasound.
Gas in the abdomen:
The images in this study are diagnostic for pneumoperitoneum as gas is clearly seen where physiological gas should not be located.
Other conditions presenting with abnormal gas that can be seen during an upper abdominal ultrasound include:
Pneumobilia, portal venous gas, emphysematous cholecystitis, cutaneous emphysema and intramuscular gas. The last two conditions will have gas superficial to the peritoneal line and are therefore not intra-abdominal gas pockets. Abnormal gas in the abdomen may be retroperitoneal as in the case of perforated retroperitoneal hollow viscera, residual air post retroperitoneal surgery or in the setting of a retroperitoneal abscess. These can be difficult to identify or differentiate on ultrasound but are easily distinguished on CT.
Being low in density causes gas to lie in antidependent positions. Therefore in the abdomen of a supine patient, it is often seen anterior to the liver. However, care must be taken as errors can be made and false-positives reported. Patients with interpositioning of the colon between the anterior abdominal wall and the liver, or gas-containing subphrenic fluid collections have been found to demonstrate an almost identical sonographic appearance as true pneumoperitoneum1. Additionally, artifacts distal to an overlying rib and the adjacent lung can mimic the appearance of free air in the abdomen2.
How to spot pneumoperitoneum
Gas is a strong reflector that appears on the ultrasound image as echogenic foci or lines depending on the size of the collection. It prevents sound transmission and generates reverberation artifact. It is often this artifact that is eye-catching and may lead the sonographer to the problem. This case study demonstrates the typical appearance of the enhanced peritoneal stripe as described by Muradali et. al1. The liver capsule may appear similarly bright to free gas, but will not result in the loss of visualisation of the underlying liver architecture3. Reverberation artifact often inhibits diagnostic information from being obtained as it obscures underlying anatomy, but in the case of a pneumoperitoneum, that appearance confirms the diagnosis.
Colour Doppler can be used as an adjunct imaging tool to increase confidence in your findings. Twinkling artifact has been found to be associated with strong reflectors that have rough surfaces such as gas bubbles4.
Scan patients supine and in the left lateral decubitus positions concentrating on the midline and right upper quadrant. You may even try scanning them erect if they are able to assume that position. Look for the enhancing peritoneal stripe with posterior reveberation artifact.
Consider using a high frequency linear transducer to better visualise these superficial structures if patient body habitus allows.
Repeated scanning of clinically suspected cases of bowel perforation is essential to detect accumulating free air over time5.
Great care must be taken to interrogate your findings, check they are reproducible, evaluate findings in conjunction with patient symptoms and consider if they fit the clinical context. As with anything in real estate and ultrasound, always think ‘location location location!’ What are you seeing, is it real, and should it be there?
DISCUSSION
This case demonstrates nicely that sometimes we are led to pathology by understanding artifact rather than spotting a mass, injury or fluid collection. Detection of free air in anatomical locations where it does not occur physiologically relies on a thorough understanding of anatomy and the physics of sound. Without paying particular care to the patient’s region of concern, optimising image settings and thinking outside the box, these small pockets of gas could have easily gone unseen and the patient may have endured many more painful weeks searching for a diagnosis and appropriate care.
The key to identifying and documenting pneumoperitonea on ultrasound is image optimisation and awareness. A poorly optimised image or an untrained eye may miss or misinterpret the common reverberation artifact from superficial structures for gas. Alternatively, they may interpret intraluminal bowel gas as being free and thus falsely diagnose a pneumoperitoneum. Erroneously reporting a pneumoperitoneum may prompt unnecessary investigations, possibly involving radiation or treatment.
This case was an uncommon presentation in a private clinic with a history of 3 weeks of pain and no trauma or recent surgery. Pneumoperitonea often present in an emergency care setting which means POCUS users need to be particularly aware of the utility of ultrasound for this condition.
Although CT remains the ‘gold-standard’, multiple studies have confirmed that ultrasound has a high sensitivity (85-100%) and high specificity (84-100%) for detecting small amounts of free intraperitoneal gas3.
When considering pneumoperitoneum as a differential, all the usual benefits of ultrasound are clear. It’s quick, cost-effective, doesn’t involve ionising radiation, and is generally well tolerated. It’s particularly helpful in situations where a patient cannot sit or stand for an erect x-ray or access to CT isn’t possible. The usual pitfalls and limitations exist also. Ultrasound is user dependent, potentially limited by patient factors (body habitus, mobility, guarding), and the quality of the equipment.
A pneumoperitoneum can have profound outcomes for the patients and has the potential to be rapidly fatal2. As this is such an important diagnosis to make, it is suggested that anyone who undertakes abdominal ultrasound should be trained in detecting pneumoperitonea.
References:
1. Muradali D, Wilson S, Burns PN, Shapiro H, Hope-Simpson D, A specific sign of pneumoperitoneum on sonography: enhancement of the peritoneal stripe. AM J Roentgenol. 1999 Nov; 173(5):1257-62.
2. Khor M, Cutten J, Lim J, Weerakkody Y. Sonographic detection of pneumoperitoneum. BJR Case Report 2017; 3: 21060146
3. A Goudie, Detection of intraperitoneal free gas by ultrasound. Australas J Ultrasound Med. 2013 May; 16(2): 56-61.
4. Kim HC, Yang DM, Jin W, Ryu JK, Shin HC, Color Doppler Twinkling Artifacts in Various Conditions During Abdominal and Pelvic Sonography. J Ultrasound Med 2010; 29:621-632.
5. Hefney AF, Abu-Zidan FM. Sonographic Diagnosis of Intraperitoneal Free Air. J Emerg Trauma Shock 2011; 4: 511-513.





